Introduction:
The chronic autoimmune disease known as rheumatoid arthritis (RA) mostly affects the joints, causing swelling, discomfort, and inflammation. Joint deterioration and diminished function may develop over time as a result of RA. RA results from the immune system mistakenly attacking healthy tissues, as opposed to osteoarthritis, which is brought on by wear and tear. Joint stiffness, exhaustion, and restricted movement are some of the signs of RA. In order to manage RA and avoid serious consequences, early diagnosis, and therapy are essential. To assist reduce symptoms and enhance the quality of life, treatment options include prescription drugs, dietary adjustments, and physical therapy.
Pathophysiology:
The immune system of the body wrongly attacks the synovium, the lining of the membranes surrounding the joints, causing rheumatoid arthritis, an inflammatory reaction. Joint discomfort and edema are brought on by this reaction’s thickening and inflammation of the synovium. The joint’s bone and cartilage may be harmed by inflammation as the illness worsens. The immune system reacts by generating inflammatory cytokines including interleukins and tumor necrosis factor-alpha (TNF-α) from cells like T cells, B cells, and macrophages. Along with causing joint degeneration and systemic symptoms like fever and exhaustion, these cytokines also sustain the inflammatory process.
Stages of Rheumatoid Arthritis:
Rheumatoid arthritis progresses through several stages, each with distinct characteristics and symptoms:
- Early Stage: Patients may experience joint stiffness, particularly in the morning, and mild joint pain and swelling. Inflammation begins in the synovium, but visible joint damage may not yet be present.
- Moderate Stage: Inflammation increases, leading to more noticeable pain, swelling, and warmth around the joints. The synovium thickens, and cartilage damage begins, reducing joint mobility and function.
- Severe Stage: Chronic inflammation results in significant cartilage and bone damage. Joints may become visibly deformed and lose alignment, leading to severe pain, considerable loss of joint function, and difficulty performing daily activities.
- End Stage: The inflammatory process may decrease, but joint damage is extensive. Joint function is severely impaired or lost, with potential complete destruction of the cartilage, bone, and joint capsule. Assistive devices or surgical interventions may be needed to manage pain and maintain mobility.
Causes of Rheumatoid Arthritis:
Rheumatoid arthritis is an autoimmune disease with a multifactorial etiology, involving genetic, environmental, and hormonal factors:
- Genetics: RA vulnerability is increased by some genes, especially those linked to the HLA-DRB1 allele. The risk is also increased by a family history of RA or other autoimmune illnesses.
- Immune System Dysfunction: When the immune system unintentionally targets the synovium, it can result in RA, which damages joints and causes chronic inflammation. It’s unclear what precisely sets off this autoimmune reaction.
- Environmental Factors: Smoking is a significant risk factor for developing RA and can worsen the disease in those already affected. Other environmental factors, such as exposure to certain bacteria or viruses, may also play a role.
- Hormonal Influences: RA is more common in women, suggesting hormonal factors, such as estrogen levels, may contribute to its development. Hormonal changes during pregnancy and menopause can also influence RA symptoms.
- Obesity: Excess body weight can increase inflammation levels and strain on joints, potentially contributing to the onset and progression of RA.
- Infections: While no specific infection has been directly linked to RA, certain infections might trigger the immune response that leads to RA in genetically predisposed individuals.
Read about osteoarthritis here.
Assessment:
To diagnose and assess the severity of rheumatoid arthritis, a thorough assessment of the patient’s symptoms, physical examination results, laboratory testing, and imaging studies are required.
- Clinical History and Symptoms
- Joint Pain and Swelling: RA usually causes discomfort, soreness, and swelling in the hands and feet tiny joints.
- Morning Stiffness: Prolonged stiffness lasting more than 30 minutes after waking is a common characteristic.
- Fatigue: Chronic fatigue and general malaise are frequently reported.
- Symmetrical Involvement: RA often affects joints symmetrically on both sides of the body.
- Physical Examination
- Joint Inspection: Swelling, redness, and warmth in the affected joints are noted.
- Palpation: Tenderness and swelling are assessed through gentle palpation.
- Range of Motion: The doctor evaluates the range of motion and looks for limitations or deformities.
- Nodules: Rheumatoid nodules, firm lumps under the skin near the joints, may be present.
- Laboratory Tests
- Rheumatoid Factor (RF): an antibody that is present in between 70 and 80 percent of RA patients.
- Anti-Cyclic Citrullinated Peptide (Anti-CCP): Highly specific for RA and can be detected early in the disease.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): Elevated levels indicate inflammation.
- Complete Blood Count (CBC): To check for anemia, which is common in RA patients.
- Imaging Studies
- X-Rays: Useful for detecting joint erosion and narrowing of joint spaces in advanced stages.
- Ultrasound: Can identify synovitis (inflammation of the synovial membrane) and fluid accumulation in early stages.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues, cartilage, and bone, and is sensitive in detecting early joint changes.
- Functional and Disability Assessment
- Health Assessment Questionnaire (HAQ): Measures physical functioning and disability.
- Patient-Reported Outcomes: Patients rate their pain, fatigue, and overall health status.
- Differential Diagnosis
- Osteoarthritis: Distinguished by the wear-and-tear nature and asymmetrical joint involvement.
- Systemic Lupus Erythematosus (SLE): Autoimmune disease with a broader range of symptoms affecting various organs.
- Gout: Characterized by sudden, severe attacks of pain due to uric acid crystal accumulation in joints.
- Ongoing Monitoring
- Regular Follow-Ups: Frequent visits to monitor symptoms and adjust treatment plans.
- Repeat Laboratory Tests and Imaging: To track inflammation levels and joint damage.
Management:
Symptom control, inflammation reduction, joint damage prevention, and general quality of life enhancement are all important aspects of managing rheumatoid arthritis.
Pharmacologic Treatments:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Purpose: Relieve pain and reduce inflammation.
- Examples: Ibuprofen, and naproxen.
- Considerations: Long-term use can cause gastrointestinal issues and cardiovascular risks.
- Corticosteroids
- Purpose: inhibit the immune system and quickly reduce inflammation.
- Examples: Prednisone.
- Considerations: Used for short-term flare control due to potential side effects like osteoporosis, weight gain, and increased infection risk.
- Disease-Modifying Antirheumatic Drugs (DMARDs)
- Purpose: Slow disease progression and prevent joint damage.
- Traditional DMARDs: Methotrexate, sulfasalazine, leflunomide, hydroxychloroquine.
- Biologic DMARDs: Specifically target immune system components (e.g., TNF inhibitors like etanercept and adalimumab).
- Janus Kinase (JAK) Inhibitors: Tofacitinib, baricitinib.
- Considerations: Regular monitoring for side effects and infection risk is essential.
Non-Pharmacologic Treatments:
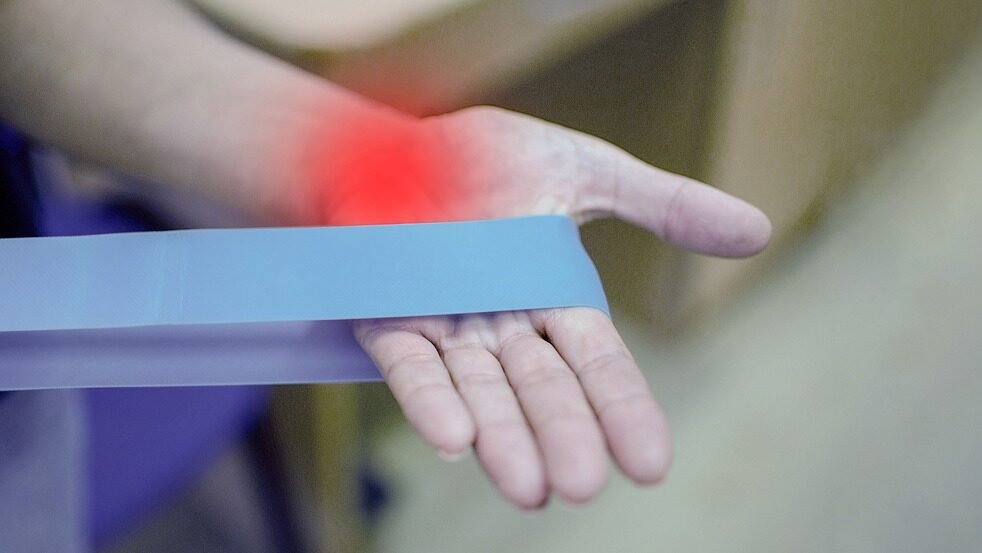
- Physical Therapy
- Purpose: Improve joint function, strength, and flexibility.
- Methods: Exercises tailored to individual needs, including range-of-motion and strengthening exercises.
- Occupational Therapy
- Purpose: Enhance the ability to perform daily activities.
- Methods: Ergonomic advice, assistive devices, and strategies to protect joints.
- Lifestyle Modifications
- Exercise: Walking and swimming are regular, low-impact exercises that help to preserve muscular strength and joint flexibility.
- Diet: Anti-inflammatory diet rich in omega-3 fatty acids, fruits, and vegetables.
- Weight Management: Maintaining a healthy weight to reduce stress on joints.
- Patient Education and Support
- Purpose: Empower patients with knowledge about RA and its management.
- Methods: Educational programs, support groups, and counseling.
Surgical Interventions:
- Joint Replacement Surgery
- Purpose: Replace severely damaged joints to improve function and relieve pain.
- Common Procedures: Hip, knee, and shoulder replacements.
- Synovectomy
- Purpose: Remove inflamed synovium to reduce pain and improve joint function.
- Method: Can be done arthroscopically.
- Tendon Repair
- Purpose: Repair tendons damaged by inflammation.
- Method: Surgical intervention to restore tendon function.
Monitoring and Ongoing Care:
- Regular Follow-Ups
- Purpose: Monitor disease activity, treatment efficacy, and side effects.
- Frequency: Typically every 3-6 months or as needed based on disease severity.
- Laboratory Tests
- Purpose: Monitor inflammation markers (ESR, CRP), liver function, kidney function, and blood counts.
- Frequency: Periodic testing based on treatment regimen.
- Imaging Studies
- Purpose: Assess joint damage and disease progression.
- Methods: X-rays, ultrasound, and MRI.
Psychological and Social Support:
- Counseling and Therapy
- Purpose: Address the emotional and psychological impact of RA.
- Methods: Cognitive-behavioral therapy, stress management techniques.
- Social Support
- Purpose: Provide a network of support from family, friends, and support groups.
- Methods: Joining RA support groups, online forums, and community resources.
Integrative and Complementary Therapies:
- Acupuncture
- Purpose: Reduce pain and improve overall well-being.
- Evidence: Some patients report benefits, though scientific evidence is mixed.
- Massage Therapy
- Purpose: Alleviate muscle tension and improve circulation.
- Considerations: This should be performed by a therapist experienced with RA patients.
- Mind-Body Techniques
- Purpose: Reduce stress and improve coping mechanisms.
- Methods: Yoga, tai chi, meditation.
Conclusion:
Pain, inflammation, and possible joint destruction are the main symptoms of rheumatoid arthritis, a chronic inflammatory disease that mostly affects the joints. To control symptoms and stop the disease from getting worse, effective care for RA entails a mix of medicines, lifestyle changes, physical and occupational therapy, and routine monitoring. To better support individuals with RA in maintaining joint function and lowering the likelihood of long-term problems, early diagnosis, and individualized treatment plans are crucial.
FAQs:
What is rheumatoid arthritis (RA)?
Rheumatoid arthritis is a long-term autoimmune disease that mostly affects the joints, producing pain, swelling, and inflammation. Over time, it may result in joint abnormalities and injury.
What options are there for treating rheumatoid arthritis?
Medication (biosimilars, painkillers, and disease-modifying antirheumatic medicines), physical therapy, dietary and lifestyle modifications, and, in extreme situations, surgery are among the available treatment options.
What are the day-to-day effects of rheumatoid arthritis?
RA can cause pain and stiffness that can make it difficult to do daily tasks like dressing, cooking, or driving, which can have an affect on daily living. Effective management can lessen these consequences.
Are there any lifestyle changes that can help manage rheumatoid arthritis?
Yes, a balanced diet, regular low-impact exercise, keeping a healthy weight, and stress management techniques can all help lessen symptoms and enhance general wellbeing.
What effects does rheumatoid arthritis have on joints?
Pain, edema, and joint deterioration are the results of inflammation in the synovial lining of the joints caused by RA. Joint abnormalities and function loss may ensue from this over time.
Can other health issues arise from rheumatoid arthritis?
Indeed, RA raises the chance of developing additional health conditions like osteoporosis, heart disease, and lung problems. To mitigate these risks, regular management and monitoring are crucial.