Introduction:
A chronic disorder called osteoporosis is characterized by a loss in bone mass and an elevated risk of fracture. It develops in porous, weak bones as a result of bone growth that does not keep up with bone resorption. Due to hormonal fluctuations, this illness primarily affects older people, especially postmenopausal women. A diet high in calcium and vitamin D, consistent weight-bearing exercise, and lifestyle modifications to reduce fall risk are examples of preventive techniques. Osteoporosis must be effectively managed and detected early to minimize its effects.
Pathophysiology:
An imbalance between the creation and resorption of bone is a characteristic of osteoporosis. In a balanced process, osteoblasts create new bone while osteoclasts tear down existing bone during bone remodeling. This equilibrium is upset in osteoporosis, which results in altered bone microarchitecture, increased bone resorption, decreased bone production, or both. Contributing factors to brittle bones prone to fractures include genetic susceptibility, insufficient nutrition, hormonal changes (particularly lowered estrogen in postmenopausal women), and physical inactivity.
Stages of Osteoporosis:
Osteoporosis progresses through several stages, each reflecting increasing bone density loss and structural compromise:
- Normal Bone Density: Bone density is within the normal range with balanced bone remodeling.
- Osteopenia: Although bone density is below average, osteoporosis cannot be diagnosed because of this. This phase is an alert system.
- Early osteoporosis: Significant bone density loss occurs, increasing fracture risk, especially in the spine, wrists, and hips. Symptoms may be absent, highlighting the need for early diagnosis.
- Established osteoporosis: Markedly reduced bone density and frequent fractures are typical. Symptoms such as back pain, loss of height, and stooped posture become apparent, with a high risk of fractures from minor falls or routine activities.
- Severe Osteoporosis: Bone density is extremely low, and fractures are common and severe, significantly impacting the quality of life due to chronic pain, disability, and fracture complications.
Causes of Osteoporosis:
Osteoporosis is primarily caused by an imbalance in bone resorption and formation when bone loss outweighs bone growth. This imbalance is caused by the following factors:
- Hormonal Changes: Bone loss is accelerated in women going through menopause by decreased estrogen levels and in men by reduced testosterone levels.
- Aging: Natural aging leads to decreased bone density as bone formation slows while resorption continues.
- Nutritional Deficiencies: Inadequate consumption of calcium and vitamin D weakens bones.
- Sedentary Lifestyle: Lack of physical activity, particularly weight-bearing and muscle-strengthening exercises, leads to weaker bones.
- Genetic Factors: A family history of osteoporosis increases the risk.
- Medical Conditions: Conditions like rheumatoid arthritis, hyperthyroidism, and gastrointestinal diseases that affect nutrient absorption increase the risk.
- Medications: Bone remodeling may be hampered by the long-term use of corticosteroids and other drugs.
- Lifestyle Choices: Bone loss is caused by smoking, drinking too much alcohol, and eating a bad diet.
Read about osteoarthritis here.
Assessment:
Assessing osteoporosis involves a comprehensive approach to evaluating bone health, identifying risk factors, and determining bone loss extent:
- Clinical History
- Medical History: Detailed medical history, including previous fractures, chronic conditions, and medications affecting bone health.
- Family History: Inquire about a family history of osteoporosis or fractures to assess genetic predisposition.
- Lifestyle Factors: Evaluation of dietary intake (calcium and vitamin D), physical activity levels, smoking, and alcohol consumption habits.
- Menstrual History: For women, information on menopause age and any history of amenorrhea affecting estrogen levels and bone density.
- Physical Examination
- Height Measurement: Comparison of current height with previous measurements to detect height loss, indicating vertebral fractures.
- Posture Assessment: Check for signs of kyphosis (forward curvature of the spine) or other postural changes suggesting vertebral fractures.
- Bone Pain and Tenderness: Evaluation of bone pain or tenderness indicating fractures or bone weakness.
- Bone Mineral Density (BMD) Testing
- DEXA Scan: The gold standard for diagnosing osteoporosis, measuring BMD at the hip and spine. Results are given as T-scores:
- Normal: T-score ≥ -1.0
- Osteopenia: T-score between -1.0 and -2.5
- Osteoporosis: T-score ≤ -2.5
- Peripheral DEXA or quantitative ultrasound is sometimes used to measure BMD at peripheral sites like the wrist, heel, or finger.
- DEXA Scan: The gold standard for diagnosing osteoporosis, measuring BMD at the hip and spine. Results are given as T-scores:
- Laboratory Tests
- Calcium and Vitamin D Levels: Assessment of serum calcium and 25-hydroxyvitamin D levels to identify deficiencies.
- Bone Turnover Markers: Assessment of indicators such as urinary N-telopeptide, osteocalcin, and serum alkaline phosphatase to measure rates of bone resorption and production.
- Hormonal Levels: Checking thyroid function (TSH), parathyroid hormone (PTH), and sex hormones (estrogen in women, testosterone in men) to identify hormonal imbalances affecting bone health.
- Secondary Causes: examinations for diseases that can lead to secondary osteoporosis, including renal function tests, CBCs, and testing for rheumatoid arthritis, celiac disease, and other pertinent disorders.
- Fracture Risk Assessment
- FRAX Tool: The 10-year chance of hip and major osteoporotic fractures is calculated using the WHO Fracture Risk Assessment Tool, which takes clinical risk factors and BMD readings into account.
- Previous Fractures: Documentation of any history of fractures, particularly those occurring with minimal trauma, significantly increasing future fracture risk.
- Additional Imaging
- Vertebral Fracture Assessment (VFA): Specialized DEXA scan detecting vertebral fractures.
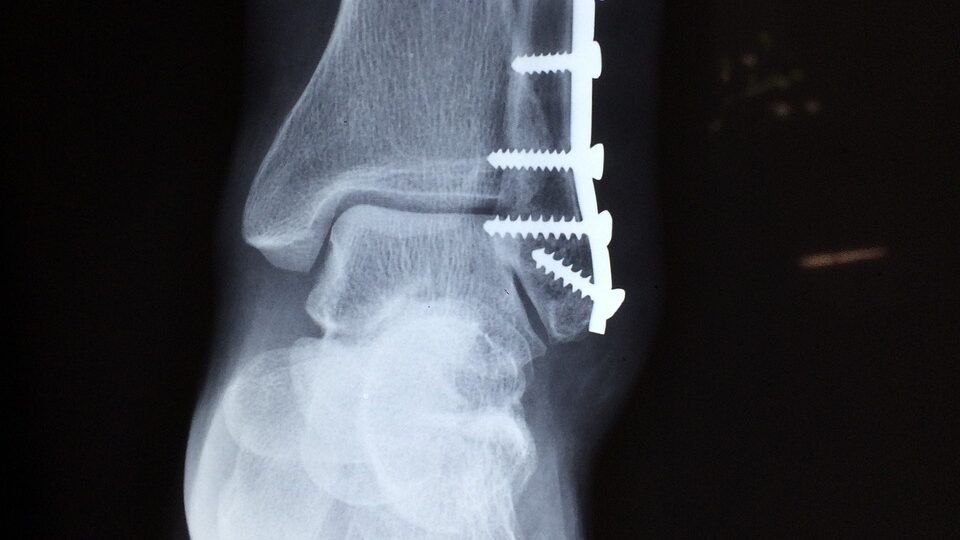
- X-rays: Used to evaluate suspected fractures, particularly in the spine.
- MRI or CT Scans: Provide detailed views of bone structure and detect subtle fractures or bone lesions in specific cases.
- Comprehensive Evaluation
- Risk Factor Analysis: Combining clinical history, physical examination, BMD results, laboratory tests, and fracture risk assessments to create a comprehensive risk profile.
- Individualized Treatment Plan: Development of a personalized treatment plan focusing on lifestyle modifications, dietary supplementation, pharmacologic interventions, and strategies to prevent falls and fractures.
Regular follow-up assessments are essential to monitor bone density, evaluate treatment effectiveness, and adjust the management plan to reduce fracture risk and improve bone health.
Management:
A comprehensive strategy is used to manage osteoporosis with the goals of reducing bone loss, boosting bone density, avoiding fractures, and enhancing general bone health:
- Lifestyle Modifications
- Nutrition: ensuring a calcium- and vitamin-D-rich diet. Fortified meals, leafy greens, and dairy products are good sources. If nutritional consumption is inadequate, supplements could be suggested.
- Exercise: frequent weight-bearing and muscle-strengthening activities to strengthen bones and improve balance, such as walking, running, and resistance training.
- Smoking Cessation: Quitting smoking, as it accelerates bone loss and increases fracture risk.
- Limiting Alcohol: Reducing alcohol intake is important, as excessive consumption can negatively impact bone health.
- Fall Prevention
- Home Safety: Modifying the living environment to reduce fall risks, including using handrails, improving lighting, and removing tripping hazards.
- Balance and Strength Training: Participating in exercises like Tai Chi and balance training will improve coordination and reduce fall risk.
- Vision and Hearing: Regular checks and corrections for vision and hearing impairments, which can contribute to falls.
- Medications
- Bisphosphonates: commonly prescribed to slow bone resorption (e.g., alendronate, risedronate, ibandronate, zoledronic acid).
- Selective Estrogen Receptor Modulators (SERMs): such as raloxifene, mimic estrogen’s protective effects on bone.
- Hormone Replacement Therapy (HRT): Estrogen therapy may be considered for postmenopausal women but must be weighed against potential risks.
- Parathyroid hormone analogs, Such as teriparatide, stimulate bone formation and are used in severe cases.
- RANK Ligand Inhibitors: Denosumab helps decrease bone resorption.
- Calcitonin: may be used in certain cases to reduce bone loss and alleviate pain from vertebral fractures.
- Monitoring and Follow-up
- Bone Density Testing: Regular DXA scans are used to monitor bone density and evaluate treatment effectiveness.
- Laboratory Tests: Periodic assessments of calcium, vitamin D levels, and other relevant biomarkers to ensure optimal bone health.
- Patient Education
- Awareness: Educating patients about the importance of bone health, adherence to medications, and lifestyle changes.
- Support Groups: Encouraging participation in support groups for emotional support and shared experiences.
- Treatment of Fractures
- Pain Management: Use of analgesics and other pain relief methods to manage discomfort from fractures.
- Surgical Intervention: In severe cases, procedures such as vertebroplasty or kyphoplasty may be necessary to stabilize fractured vertebrae.
- Addressing Secondary Causes
- Medical Evaluation: Treating underlying conditions that may contribute to osteoporosis, such as thyroid disorders or gastrointestinal diseases affecting nutrient absorption.
Conclusion:
Osteoporosis management requires a comprehensive approach, combining lifestyle modifications, fall prevention strategies, pharmacologic interventions, and regular monitoring. Early diagnosis and effective treatment are crucial to preventing fractures, maintaining bone health, and improving the quality of life for individuals with osteoporosis.
FAQs:
What is osteoporosis?
Osteoporosis is a disorder in which bones are weaker and more prone to fractures. It occurs when bone density and quality decrease.
What are some typical causes of osteoporosis?
Osteoporosis can be caused by aging, hormonal changes (particularly in postmenopausal women), insufficient calcium and vitamin D intake, sedentary lifestyle, and some drugs.
How is osteoporosis diagnosed?
Osteoporosis is often detected via bone density tests, such as Dual-energy X-ray Absorptiometry (DEXA) scans, which evaluate mineral content in bones.
What symptoms of osteoporosis are present?
Many times, osteoporosis is asymptomatic until a fracture happens. On the other hand, a hunched posture, progressive height reduction, and back pain are other symptoms.
Are males at risk of osteoporosis?
Absolutely, although osteoporosis is more frequent in women, males can also get it, especially if they have risk factors like low testosterone, steroid usage, or a family history of the disease.
Can osteoporosis be inherited?
Genetics can influence osteoporosis; a family history of the disorder raises the risk. Lifestyle choices, however, also play a big role.
Is osteoporosis contagious?
Osteoporosis is not contagious. It cannot be transferred from one person to another via touch, air, or any other channel.
What steps can I take to lower my chance of osteoporosis?
By eating a balanced diet high in calcium and vitamin D, exercising regularly with weights, abstaining from smoking, and consuming alcohol in moderation, you can lower your risk.


2 thoughts on “Osteoporosis: Pathophysiology and Breakthrough Solutions”