Introduction:
Cervical spondylosis, or neck arthritis, is an age-related degeneration of cervical spine joints and discs. Symptoms include chronic neck pain, stiffness, headaches, and, in severe cases, numbness or weakness in the arms. Diagnosis involves physical exams and imaging. Treatments include medication, physical therapy, injections, and surgery for severe cases. Prevention focuses on exercise, good posture, and avoiding strain. With proper management, individuals can alleviate symptoms and maintain quality of life.

Pathophysiology:
Cervical spondylosis develops as the cervical spine undergoes degenerative changes over time. Initially, the intervertebral discs lose water content and elasticity, becoming stiff and less able to absorb shocks. This leads to microtrauma and small tears in the annulus fibrosus. As the discs degenerate, there is increased stress on the facet joints, causing them to hypertrophy and develop osteophytes (bone spurs). These changes can narrow the neural foramina and spinal canal, compressing nerve roots or the spinal cord. In response, the body may form new bone around the degenerating discs and joints, exacerbating symptoms like pain, stiffness, and neurological deficits.
Stages or Phases of Cervical Spondylosis:
Cervical spondylosis generally progresses through several stages or phases:
- Initial Degeneration: The intervertebral discs lose water content and elasticity, becoming stiff. This phase may not cause symptoms but sets the stage for further degeneration.
- Development of Osteophytes: As degeneration progresses, bone spurs (osteophytes) may form around the edges of vertebrae and facet joints, contributing to stiffness and pain.
- Narrowing of Spinal Canal: Degenerative changes can lead to the narrowing of the spinal canal (spinal stenosis) or neural foramina, potentially compressing spinal nerves or the spinal cord.
- Advanced Degeneration: In severe cases, discs may collapse, and there can be significant loss of disc height and joint space, leading to more pronounced symptoms such as radiculopathy (pain radiating down the arms) or myelopathy (spinal cord compression).
Age, way of life, and the existence of underlying medical disorders are some of the variables that might affect how cervical spondylosis progresses in different people. It is possible to lessen symptoms and halt development with consistent monitoring and effective care.
Read about cervical radiculopathy here.
Causes:
The primary causes of cervical spondylosis include:
- Age: Degenerative changes in the spine are a natural part of aging.
- Wear and Tear: Repetitive movements or activities that strain the neck over time.
- Genetics: Family history can predispose individuals to develop cervical spine problems.
- Previous Neck Injuries: Trauma or accidents that affect the cervical spine.
- Occupational Factors: Jobs or activities that involve repetitive neck movements, heavy lifting, or poor ergonomics.
- Smoking: Tobacco use has been linked to increased cervical spine degeneration.
These factors contribute to the gradual breakdown of discs, joints, and ligaments in the neck, leading to cervical spondylosis.
Assessment:
Physical Therapy
In physical therapy, cervical spondylosis is assessed using a comprehensive approach that aims to identify and meet each patient’s specific requirements.
- Initial Evaluation:
- Clinical Assessment: Includes a detailed history and physical examination to assess symptoms such as neck pain, stiffness, and neurological deficits. Palpation helps identify tender areas, while functional tests evaluate how symptoms impact daily activities.
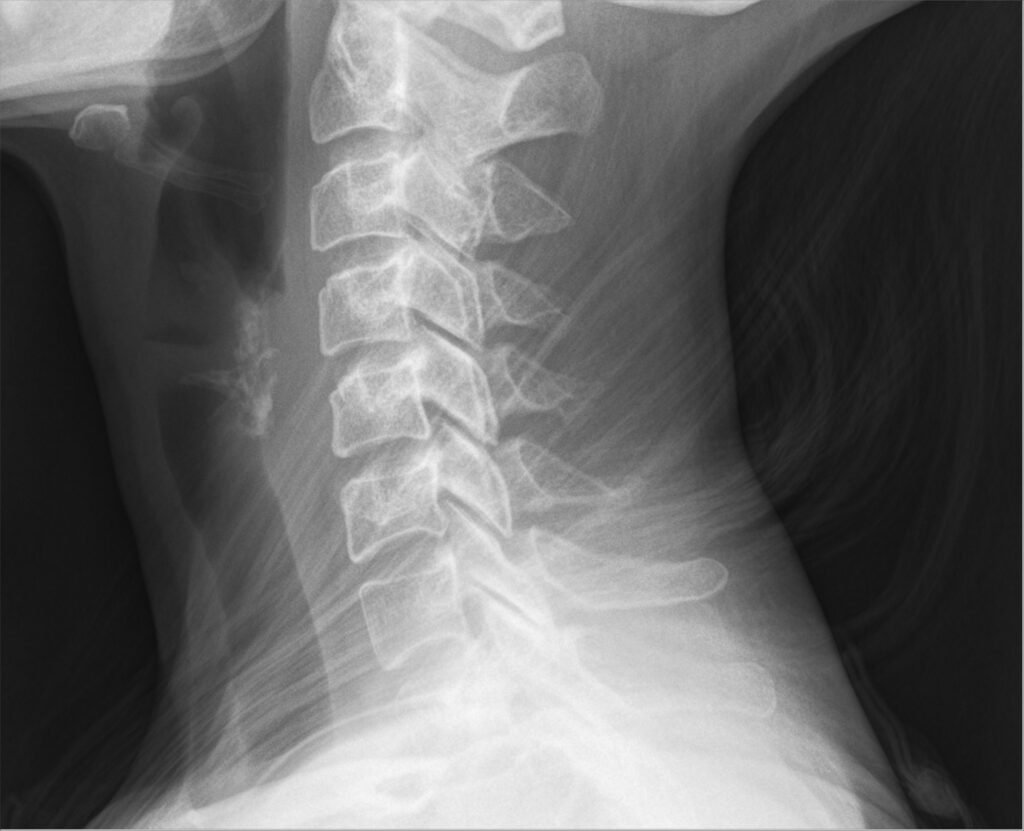
- Diagnostic Imaging: X-rays, MRI scans, or CT scans may be used to visualize structural changes in the cervical spine, such as degenerated discs, osteophytes, or spinal stenosis.
- Functional Impairments:
- Assessment of range of motion limitations and muscle strength deficits related to cervical spine dysfunction.
- Evaluation of posture and biomechanics to identify contributing factors and ergonomic issues.
- Treatment Planning:
- Exercise Prescription: Individualized exercise programs focus on improving neck mobility, strengthening muscles that support the cervical spine, and enhancing overall flexibility. Exercises may include stretching, strengthening, and stabilization techniques.
- Manual Therapy: Techniques such as joint mobilizations and soft tissue mobilizations are used to alleviate pain, improve range of motion, and restore joint function.
- Modalities: Heat, cold, ultrasound, or electrical stimulation may be applied to reduce pain and inflammation.
- Education: Patient education on posture correction, ergonomics, and strategies to manage symptoms during daily activities.
- Progress Monitoring:
- Regular reassessment of symptoms, functional status, and treatment goals is necessary to track progress and modify therapy as needed.
- Collaboration with other healthcare professionals, such as physicians or occupational therapists, to optimize patient care and outcomes.
- Long-term Management:
- Emphasis on self-management strategies and home exercise programs to maintain improvements achieved during therapy.
- Periodic follow-ups to monitor for recurrence of symptoms or progression of cervical spondylosis.
Physical therapists work to restore function, reduce discomfort, and improve the quality of life for patients with cervical spondylosis by using a multifaceted evaluation approach and customized therapy plans.
General Assessment of Cervical Spondylosis
Cervical spondylosis assessment encompasses a thorough evaluation to understand the condition’s impact and guide appropriate management:
1. History Taking:
- Detailed inquiry into symptoms such as neck pain, stiffness, headaches, and any radiating arm pain.
- Exploration of factors exacerbating or alleviating symptoms, including past injuries or familial predisposition.
3. Imaging Studies:
- X-rays provide an initial assessment of structural changes like osteophytes (bone spurs) and narrowing of disc spaces.
- MRI or CT scans offer detailed views of soft tissues, discs, and neural structures to confirm diagnosis and assess severity.
4. Functional Assessment:
- Evaluation of how symptoms affect daily activities, work-related tasks, and quality of life.
- Assessment of posture and ergonomic factors contributing to symptoms.
5. Diagnostic Considerations:
- Differential diagnosis is used to rule out other conditions causing similar symptoms, such as cervical disc herniation or spinal stenosis.
6. Psychological and Social Factors:
- Consideration of psychological stressors or comorbidities impacting symptom perception and management.
- Assessment of social support systems and lifestyle factors influencing treatment adherence and outcomes.
7. Collaborative Approach:
- Coordination with multidisciplinary teams, including physical therapists, physicians, and specialists, to develop a comprehensive treatment plan.
- Patient education on the nature of cervical spondylosis, treatment options, and strategies for symptom management and prevention.
A holistic assessment helps tailor interventions to alleviate pain, improve function, and enhance overall well-being for individuals with cervical spondylosis.
Comprehensive Management of Cervical Spondylosis:
General management of cervical spondylosis involves a holistic approach to alleviate symptoms and improve overall function:
- Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and analgesics to manage pain and inflammation.
- Physical Therapy: Exercises to strengthen neck muscles, improve flexibility, and correct posture. Manual therapy such as joint mobilizations and soft tissue techniques can also help.
- Lifestyle Modifications: Ergonomic adjustments at work and home, proper posture techniques, and avoiding activities that strain the neck.
- Modalities: Heat or cold therapy, ultrasound, and electrical stimulation to reduce pain and improve muscle function.
- Surgery: Reserved for severe cases with significant nerve compression or spinal cord involvement.
- Education and Self-management: Understanding the condition, adhering to treatment plans, and adopting healthy habits like regular exercise and weight management.
- Regular Monitoring: Periodic assessments to track progress, adjust treatments, and prevent complications.
By combining these strategies, individuals can effectively manage cervical spondylosis and maintain a good quality of life.
Management of Cervical Spondylosis with Physical Therapy
Effective management of cervical spondylosis involves a multifaceted approach, with physical therapy playing a central role in alleviating symptoms and improving function:
1. Exercise Therapy:
- Stretching Exercises: Targeted stretches for the neck muscles help improve flexibility and reduce stiffness.
- Strengthening Exercises: Progressive resistance exercises for the neck and shoulder muscles enhance support for the cervical spine.
- Stabilization Exercises: Core strengthening exercises to improve posture and stability, reducing strain on the neck.
2. Manual Therapy:
- Joint Mobilizations: Gentle movements are applied to the cervical spine joints to reduce pain, improve range of motion, and restore function.
- Soft Tissue Mobilizations: Techniques such as massage or myofascial release to alleviate muscle tension and improve tissue flexibility.
3. Modalities:
- Heat Therapy: Application of heat packs or warm towels to increase blood flow, relax muscles, and reduce pain and stiffness.
- Cold Therapy: Cold packs or ice are applied to numb sore tissues and reduce inflammation.
- Electrical Stimulation: Transcutaneous electrical nerve stimulation (TENS) or ultrasound helps to relieve pain and promote healing.
4. Posture Education and Ergonomics:
- Instruction on proper posture during daily activities, sitting, standing, and sleeping to reduce strain on the cervical spine.
- Ergonomic assessment and modifications in workplace or home settings to optimize neck alignment and reduce repetitive strain.
5. Patient Education:
- Understanding the condition, its causes, and factors that exacerbate symptoms.
- Teaching self-management strategies, including exercises, posture correction, and ergonomic principles for long-term symptom control.
6. Behavioral Modifications:
- Encouraging lifestyle changes such as smoking cessation and weight management to reduce additional stress on the cervical spine.
- Stress management techniques to alleviate muscle tension and promote relaxation.
7. Graduated Return to Activities:
- Guiding patients through a gradual return to normal activities and sports, ensures they understand limitations and techniques to prevent re-injury.
8. Continual Assessment and Adjustment:
- Regular reassessment of symptoms, functional status, and treatment goals to modify therapy plans as needed for optimal outcomes.
- Collaboration with other healthcare professionals, such as physicians or occupational therapists, for comprehensive care.
Physical therapy for cervical spondylosis aims to reduce pain, improve neck function, and enhance quality of life by addressing underlying impairments and promoting long-term management strategies.
Conclusion:
In conclusion, cervical spondylosis, characterized by age-related degeneration of the cervical spine, presents with symptoms like chronic neck pain and stiffness. Effective management involves a comprehensive approach including physical therapy, medication, and possibly surgery for severe cases. Assessment through clinical exams and imaging guides personalized treatment plans aimed at reducing pain, improving function, and enhancing quality of life. By emphasizing exercise, posture correction, and ergonomic adjustments, individuals can mitigate symptoms and prevent progression. With proper care, those affected can maintain independence and manage symptoms effectively over time.
FAQs:
What is cervical spondylosis?
Degeneration of the cervical spine’s (neck region’s) discs and vertebrae is the hallmark of cervical spondylosis, a disorder that frequently causes pain, stiffness, and other symptoms.
What are the causes of cervical spondylosis?
Age-related degeneration of the spine, fluid loss and deterioration of the spinal discs, formation of bone spurs surrounding the discs, and herniated discs are the main reasons.
What stages does cervical spondylosis go through?
Stages are generally classified according to the degree of degeneration and the existence of symptoms, ranging from mild to severe. Advanced stages might result in severe nerve compression and problems with mobility, while early stages may just cause mild discomfort and stiffness.
Is it possible to avoid cervical spondylosis?
Cervical spondylosis can be prevented by keeping proper posture, engaging in neck exercises, quitting smoking, and implementing ergonomic measures, even though age-related deterioration is a common cause.
What changes to one’s lifestyle can assist control of cervical spondylosis?
Keeping a healthy weight, adopting proper posture, making use of ergonomic furniture and equipment, exercising when appropriate, controlling stress, and keeping physically active can all help with symptom management and quality of life enhancement.


1 thought on “A Comprehensive Guide to Cervical Spondylosis: Stages, Causes, and Treatments”